News
Original reporting, exclusive interviews, and sharp analysis by experienced journalists. Coverage of the breaking and developing news that IT executives need to know about, like moves in the enterprise IT market, major cyberattacks, and more.
Technologist and author Bruce Schneier addresses the crowd at RSA Conference 2024 about the future impacts of AI on democracy.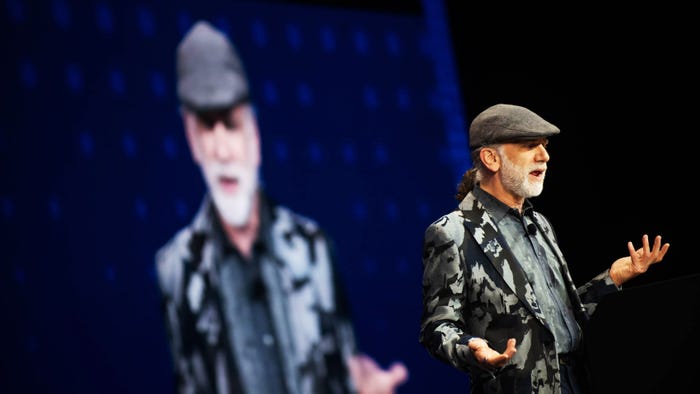
Machine Learning & AI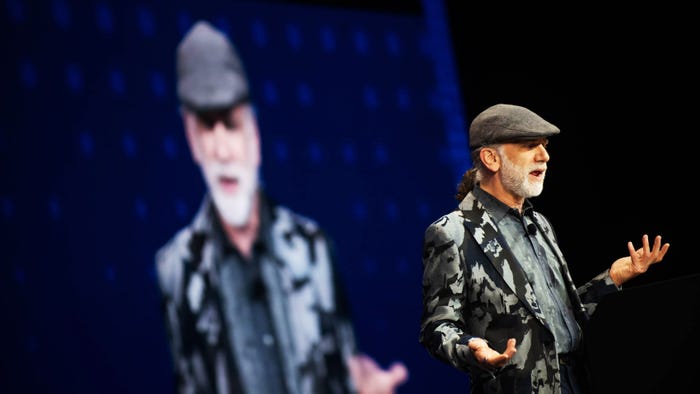
Bruce Schneier: 5 Ways AI Could Shake Up DemocracyBruce Schneier: 5 Ways AI Could Shake Up Democracy
The renowned technologist and author details the good, bad, and ugly possibilities of artificial intelligence and its impact on everything from politics to law.
Never Miss a Beat: Get a snapshot of the issues affecting the IT industry straight to your inbox.























.jpg?width=300&auto=webp&quality=80&disable=upscale)