News
Original reporting, exclusive interviews, and sharp analysis by experienced journalists. Coverage of the breaking and developing news that IT executives need to know about, like moves in the enterprise IT market, major cyberattacks, and more.
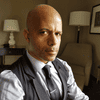
FBI Director Christopher Wray testifies during a Senate Intelligence Committee Hearing on worldwide threats on Capitol Hill in Washington, DC 
Cyber Resilience
The Continuing Vulnerability of US Critical InfrastructureThe Continuing Vulnerability of US Critical Infrastructure
FBI Director Christopher Wray called for collaboration to protect critical infrastructure from Chinese government cyber threats.
Never Miss a Beat: Get a snapshot of the issues affecting the IT industry straight to your inbox.
















.jpg?width=300&auto=webp&quality=80&disable=upscale)




















.jpg?width=300&auto=webp&quality=80&disable=upscale)






